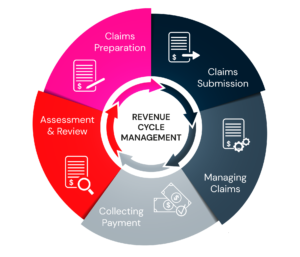
End to End Revenue Cycle Management Services
We work as an extension of you medical billing company and provide end-to-end services such as – Appointment Scheduling, Patient Demographics, Eligibility Verification, Prior Authorization, Coding, Charge Entry, Claim Submission, AR Follow-up, Denial Management, Payment Posting, Patient Billing Support and Provider Credentialing.